The most exciting development of the twentieth century has been the development of myoelectric prosthetic limbs. Myoelectricity involves using electrical signals from the patient’s arm muscles to move the limb

Background
Artificial arms and legs, or prostheses, are intended to restore a degree of normal function to amputees. Mechanical devices that allow amputees to walk again or continue to use two hands have probably been in use since ancient times, the most notable one being the simple peg leg. Surgical procedure for amputation, however, was not largely successful until around 600 B.C. Armorers of the Middle Ages created the first sophisticated prostheses, using strong, heavy, inflexible iron to make limbs that the amputee could scarcely control. Even with the articulated joints invented by Ambroise Pare in the 1500s, the amputee could not flex at will. Artificial hands of the time were quite beautiful and intricate imitations of real hands, but were not exceptionally functional. Upper limbs, developed by Peter Baliff of Berlin in 1812 for below-elbow amputees and Van Peetersen in 1844 for above-elbow amputees, were functional, but still far less than ideal.
The nineteenth century saw a lot of changes, most initiated by amputees themselves. J. E. Hanger, an engineering student, lost his leg in the Civil War. He subsequently designed an artificial leg for himself and in 1861 founded a company to manufacture prosthetic legs. The J. E. Hanger Company is still in existence today. Another amputee named A. A. Winkley developed a slip-socket below-knee device for himself, and with the help of Lowell Jepson, founded the Winkley Company in 1888. They marketed the legs during the National Civil War Veterans Reunion, thereby establishing their company.
Another amputee named D. w. Dorrance invented a terminal device to be used in the place of a hand in 1909. Dorrance, who had lost his right arm in an accident, was unhappy with the prosthetic arms then available. Until his invention, they had consisted of a leather socket and a heavy steel frame, and either had a heavy cosmetic hand in a glove, a rudimentary mechanical hand, or a passive hook incapable of prehension. Dorrance invented a split hook that was anchored to the opposite shoulder and could be opened with a strap across the back and closed by rubber bands. His terminal device (the hook) is still considered to be a major advancement for amputees because it restored their prehension abilities to some extent. Modified hooks are still used today, though they might be hidden by realistic- looking skin.
The twentieth century has seen the greatest advances in prosthetic limbs. Materials such as modern plastics have yielded prosthetic devices that are strong and more lightweight than earlier limbs made of iron and wood. New plastics, better pigments, and more sophisticated procedures are responsible for creating fairly realistic-looking skin.
The most exciting development of the twentieth century has been the development of myoelectric prosthetic limbs. Myoelectricity involves using electrical signals from the patient’s arm muscles to move the limb. Research began in the late 1940s in West Germany, and by the late sixties myoelectric devices were available for adults. In the last decade children have also been fitted with myoelectric limbs.
In recent years computers have been used to help fit amputees with prosthetic limbs. Eighty-five percent of private prosthetic facilities use a CAD/CAM to design a model of the patient’s arm or leg, which can be used to prepare a mold from which the new limb can be shaped. Laser-guided measuring and fitting is also available.
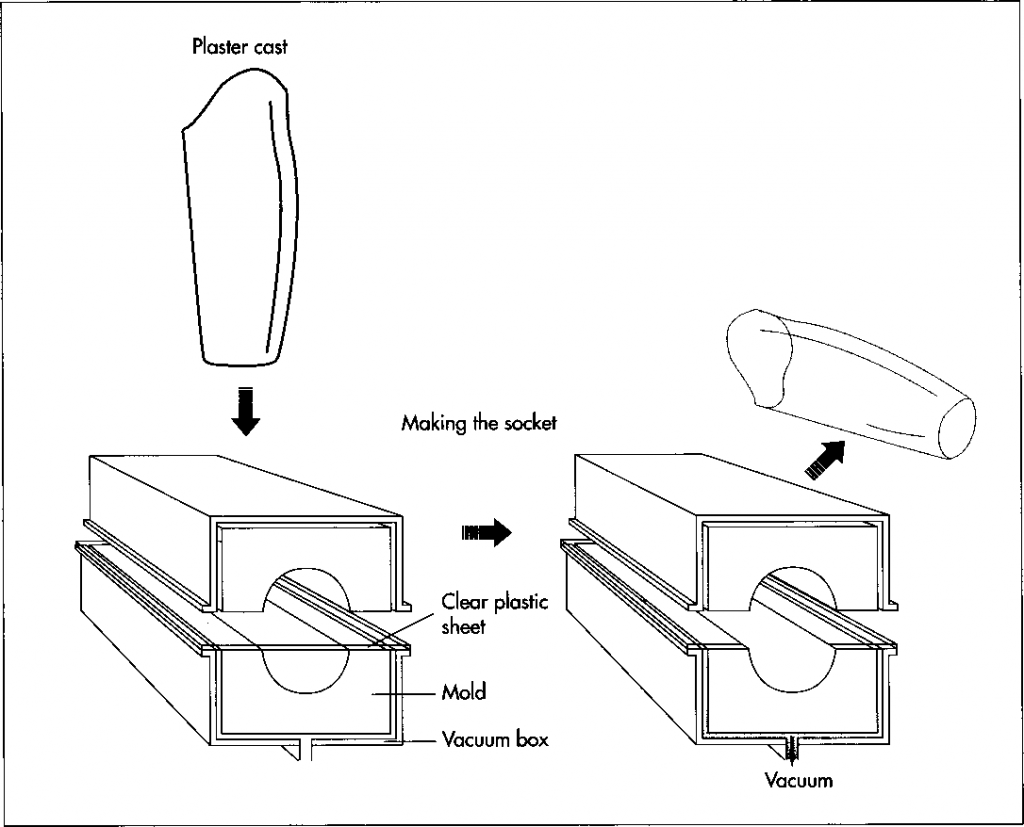
After a plaster cast of the amputee’s stump is made, a thermoplastic sheet is vacuum-formed around this cast to form a test socket. In vacuum-forming, the plastic sheet is healed and then placed in a vacuum chamber with the cast (or mold). As the air is sucked out of the chamber, the plastic adheres to the cast and assumes its shape. After testing, the permanent socket is formed in the same way.
Raw Materials
The typical prosthetic device consists of a custom fitted socket, an internal structure (also called a pylon), knee cuffs and belts that attach it to the body, prosthetic socks that cushion the area of contact, and, in some cases, realistic-looking skin. Prosthetic limb manufacture is currently undergoing changes on many levels, some of which concern the choice of materials.
A prosthetic device should most of all be lightweight; hence, much of it is made from plastic. The socket is usually made from polypropylene. Lightweight metals such as titanium and aluminum have replaced much of the steel in the pylon. Alloys of these materials are most frequently used. The newest development in prosthesis manufacture has been the use of carbon fiber to form a lightweight pylon.
Certain parts of the limb (for example, the feet) have traditionally been made of wood (such as maple, hickory basswood, willow, poplar, and linden) and rubber. Even today the feet are made from urethane foam with a wooden inner keel construction. Other materials commonly used are plastics such as polyethylene, polypropylene, acrylics, and polyurethane. Prosthetic socks are made from a number of soft yet strong fabrics. Earlier socks were made of wool, as are some modem ones, which can also be made of cotton or various synthetic materials.
Physical appearance of the prosthetic limb is important to the amputee. The majority of endoskeletal prostheses (pylons) are covered with a soft polyurethane foam cover that has been designed to match the shape of the patient’s sound limb. This foam cover is then covered with a sock or artificial skin that is painted to match the patient’s skin color.
The Manufacturing Process
Prosthetic limbs are not mass-produced to be sold in stores. Similar to the way dentures or eyeglasses are procured, prosthetic limbs are first prescribed by a medical doctor, usually after consultation with the amputee, a prosthetist, and a physical therapist. The patient then visits the prosthetist to be fitted with a limb. Although some parts—the socket, for instance—are custom-made, many parts (feet, pylons) are manufactured in a factory, sent to the prosthetist, and assembled at the prosthetist’s facility in accordance with the patient’s needs. At a few facilities, the limbs are custom made from start to finish.
Measuring and casting
1 Accuracy and attention to detail are important in the manufacture of prosthetic limbs, because the goal is to have a limb that comes as close as possible to being as comfortable and useful as a natural one. Before work on the fabrication of the limb is begun, the prosthetist evaluates the amputee and takes an impression or digital reading of the residual limb.
2 The prosthetist then measures the lengths of relevant body segments and determines the location of bones and tendons in the remaining part of the limb. Using the impression and the measurements, the prosthetist then makes a plaster cast of the stump. This is most commonly made of plaster of paris, because it dries fast and yields a detailed impression. From the plaster cast, a positive model—an exact duplicate—of the stump is created.
Making the socket
3 Next, a sheet of clear thermoplastic is heated in a large oven and then vacuum- formed around the positive mold. In this process, the heated sheet is simply laid over the top of the mold in a vacuum chamber. If necessary, the sheet is heated again. Then, the air between the sheet and the mold is sucked out of the chamber, collapsing the sheet around the mold and forcing it into the exact shape of the mold. This thermoplastic sheet is now the test socket; it is transparent so that the prosthetist can check the fit.
4 Before the permanent socket is made, the prosthetist works with the patient to ensure that the test socket fits properly. In the case of a missing leg, the patient walks while wearing the test socket, and the prosthetist studies the gait. The patient is also asked to explain how the fit feels; comfort comes first. The test socket is then adjusted according to patient input and retried. Because the material from which the test socket is made is thermoplastic, it can be reheated to make minor adjustments in shape. The patient can also be fitted with thicker socks for a more comfortable fit.
5 The permanent socket is then formed. Since it is usually made of polypropylene, it can be vacuum-formed over a mold in the same way as the test socket. It is common for the stump to shrink after surgery, stabilizing approximately a year later. Thus, the socket is usually replaced at that time, and thereafter when anatomical changes necessitate a change.
Fabrication of the prosthesis
6 There are many ways to manufacture the parts of a prosthetic limb. Plastic pieces—including soft-foam pieces used as liners or padding—are made in the usual plastic forming methods. These include vacuum- forming (see no. 3 above), injecting molding —forcing molten plastic into a mold and letting it cool—and extruding, in which the plastic is pulled through a shaped die. Pylons that are made of titanium or aluminum can be die-cast; in this process, liquid metal is forced into a steel die of the proper shape. The wooden pieces can be planed, sawed, and drilled. The various components are put together in a variety of ways, using bolts, adhesives, and laminating, to name a few.
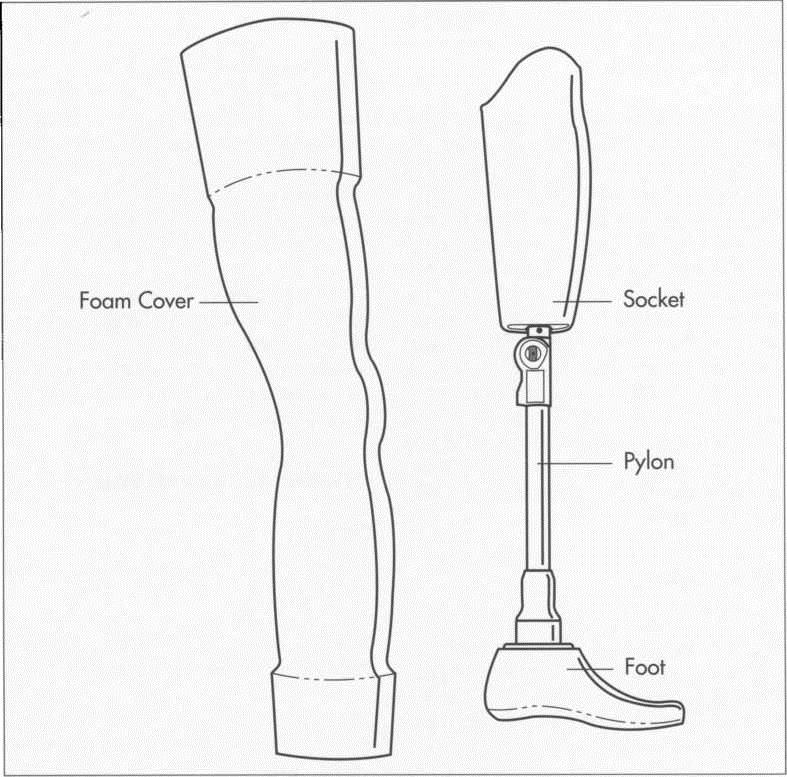
A typical artificial limb, in this case an above-the-knee prosthesis. The foam cover is covered with artificial skin that is painted to match the patient’s natural skin color.
7 The entire limb is assembled by the prosthetist’s technician using such tools as a prosthetic device together. After this, the prosthetist again fits the permanent socket to the patient, this time with the completed custom-made limb attached. Final adjustments are then made.
Physical Therapy
Once the prosthetic limb has been fitted, it is necessary for the patient to become comfortable with the device and learn to use it in order to meet the challenges of everyday life. At the same time, they must learn special exercises that strengthen the muscles used to move the prosthetic device. When the patient has been fitted with a myoelectric device, it is sometimes true that the muscles are too weak to effectively signal the device, so again the muscles are exercised to strengthen them. Some new amputees are trained to wash the devices—including the socks— daily, and to practice getting them on and off.
A patient fitted with an artificial arm must learn to use the arm and its locking device as well as the hand. If the amputee lost an arm due to an accident and is subsequently fitted with a myoelectric device, this is relatively easy. If the loss of the limb is congenital, this is difficult. An instruction system has been developed to teach amputees how to accomplish many small tasks using only one hand.
Some patients fitted with an artificial leg also undergo physical therapy. It typically takes a new amputee 18-20 weeks to learn how to walk again. Patients also learn how to get in and out of bed and how to get in and out of a car. They learn how to walk up and down hill, and how to fall down and get up safely.
Quality Control
No standards exist for prosthetic limbs in the United States. Some manufacturers advocate instituting those of the International Standards Organization of Europe, particularly because U.S. exporters of prosthetic limbs to Europe must conform to them anyway.
A typical artificial limb, in this case an above-the-knee prosthesis. The foam cover is covered with artificial skin that is painted to match the patient’s natural skin color.
Others believe these regulations to be confusing and unrealistic; they would rather see the United States produce their own, more reasonable standards.
Lack of standards does not mean that prosthetic limb manufacturers have not come up with ways to test their products. Some tests evaluate the strength and lifetime of the device. For instance, static loads test strength. A load is applied over a period of 30 seconds, held for 20 seconds, then removed over a period of 30 seconds. The limb should suffer no deformation from the test. To test for failure, a load is applied to the limb until it breaks, thus determining strength limits. Cyclic loads determine the lifetime of the device. A load is applied two million times at one load per second, thus simulating five years of use. Experimental prosthetic limbs are usually considered feasible if they survive 250,000 cycles.
The Future
Many experts are optimistic about the future of prosthetic limbs; at least, most agree that there is vast room for improvement. A prosthetic limb is a sophisticated device, yet it is preferably simple in design. The ideal prosthetic device should be easy for the patient to learn how to use, require little repair or replacement, be comfortable and easy to put on and take off, be strong yet lightweight, be easily adjustable, look natural, and be easy to clean. Research aims for this admittedly utopian prosthetic device, and strides have been made in recent years.
Carbon fiber is a strong, lightweight material that is now being used as the basis of endoskeletal parts (the pylons). In the past it was used primarily for reinforcement of exoskeletal protheses, but some experts claim that carbon fiber is a superior material that will eventually replace metals in pylons.
One researcher has developed software that superimposes a grid on a CAT scan of the stump to indicate the amount of pressure the soft tissue can handle with a minimum amount of pain. By viewing the computer model, the prosthetist can design a socket that minimizes the amount of soft tissue that is displaced.
An experimental pressure-sensitive foot is also in the works. Pressure transducers located in the feet send signals to electrodes set in the stump. The nerves can then receive and interpret the signals accordingly. Amputees can walk more normally on the new device because they can feel the ground and adjust their gait appropriately.
Another revolutionary development in the area of prosthetic legs is the introduction of an above-knee prosthesis that has a built-in computer that can be programmed to match the patient’s gait, thereby making walking more automatic and natural.
Where To Learn More
Books
Forester, C. S. Flying Colours. Little, Brown, 1938.
Sabolich, John. You ’re Not Alone. Sabolich Prosthetic and Research Center, 1991.
Shurr, Donald G. and Thomas M. Cook. Prosthetics and Orthotics. Appleton and Lange, 1990.
Periodicals
Abrahams, Andrew. “An Amazing ‘Foot’ Puts Legless Vet Bill Demby Back in the Ballgame,” People Weekly. April 4, 1988, p. 119.
Hart, Lianne. “Lives that Are Whole,” Life. December, 1988, pp. 112-116.
Heilman, Joan Rattner. “Medical Miracles,” Redbook. May, 1991, p. 124+.
“A Helping Hand for Christa,” National Geographic World. November, 1986, p. 10.